Understanding Sclerotherapy
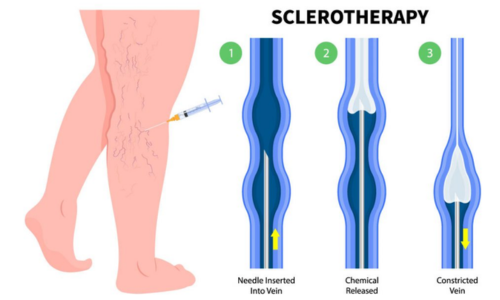
Sclerotherapy is a minimally invasive procedure used to treat varicose veins, hemorrhoids, and certain vascular malformations. In gastroenterology, sclerotherapy is commonly performed to treat esophageal varices, which are enlarged and swollen veins in the esophagus that can lead to life-threatening bleeding. During sclerotherapy, a sclerosing agent is injected directly into the affected veins, causing them to shrink, collapse, and eventually be absorbed by the body.
Procedure Overview
During a sclerotherapy procedure for esophageal varices:
- Preparation: Before the procedure, patients may receive sedation or anesthesia to help them relax and minimize discomfort.
- Endoscopic Guidance: The gastroenterologist uses an endoscope inserted through the mouth to visualize the esophageal varices.
- Injection of Sclerosing Agent: Using a specialized needle passed through the endoscope, a sclerosing agent (such as ethanolamine or sodium tetradecyl sulfate) is injected directly into the varices. The sclerosing agent causes inflammation and scarring of the vein walls, leading to their closure and eventual resolution.
- Monitoring: Patients are monitored closely for any signs of bleeding, complications, or adverse reactions to the sclerosing agent.
- Repeat Sessions: Multiple sclerotherapy sessions may be required to fully treat all varices and reduce the risk of recurrent bleeding.
- Follow-up: Patients may require regular follow-up appointments to assess the effectiveness of the treatment and monitor for recurrence of varices or complications.
Uses and Benefits of Sclerotherapy
Sclerotherapy is used for:
- Treatment of Esophageal Varices: Sclerotherapy helps reduce the size and pressure of esophageal varices, minimizing the risk of variceal bleeding and improving outcomes in patients with liver cirrhosis or portal hypertension.
- Prevention of Variceal Bleeding: By inducing sclerosis and closure of the varices, sclerotherapy helps prevent or minimize the risk of variceal hemorrhage, which can be life-threatening.
- Minimally Invasive: Sclerotherapy is performed endoscopically, without the need for surgery or major incisions, resulting in shorter recovery times and reduced risk of complications.
- Long-term Management: Sclerotherapy is an effective long-term treatment for esophageal varices, reducing the risk of recurrent bleeding and improving quality of life for patients with liver cirrhosis or portal hypertension.
- Improved Prognosis: By reducing the risk of variceal bleeding and its associated complications, sclerotherapy can improve overall prognosis and survival rates in patients with advanced liver disease.
Indications for Video Gastroduodenoscopy
Video Gastroduodenoscopy may be recommended for patients experiencing symptoms such as:
- Difficulty Swallowing: Persistent difficulty swallowing (dysphagia) or pain with swallowing (odynophagia).
- Upper Abdominal Pain: Chronic or recurrent upper abdominal pain, discomfort, or bloating.
- Gastrointestinal Bleeding: Evidence of gastrointestinal bleeding, such as black, tarry stools (melena) or bloody vomit (hematemesis).
- Unexplained Weight Loss: Significant or unexplained weight loss despite normal eating habits.
- Reflux Symptoms: Symptoms of gastroesophageal reflux disease (GERD), such as heartburn, regurgitation, or chest pain.
- Screening or Surveillance: Routine screening or surveillance for conditions such as Barrett's esophagus, esophageal varices, or gastric polyps.
Conclusion
Sclerotherapy is a valuable therapeutic procedure used to treat esophageal varices and prevent variceal bleeding in patients with liver cirrhosis or portal hypertension. By inducing sclerosis and closure of the varices, sclerotherapy helps reduce the risk of bleeding and improve outcomes for individuals at risk of variceal hemorrhage.